Gastroparesis is a condition that affects the stomach’s ability to properly empty its contents. It can lead to various symptoms and complications that affect a person’s quality of life. In this article, we will explore the causes of gastroparesis, its symptoms, available treatments, dietary recommendations, and how it relates to conditions like irritable bowel disease (IBD) and multiple sclerosis (MS).
Table of Contents
ToggleGastroparesis Meaning: What is It?
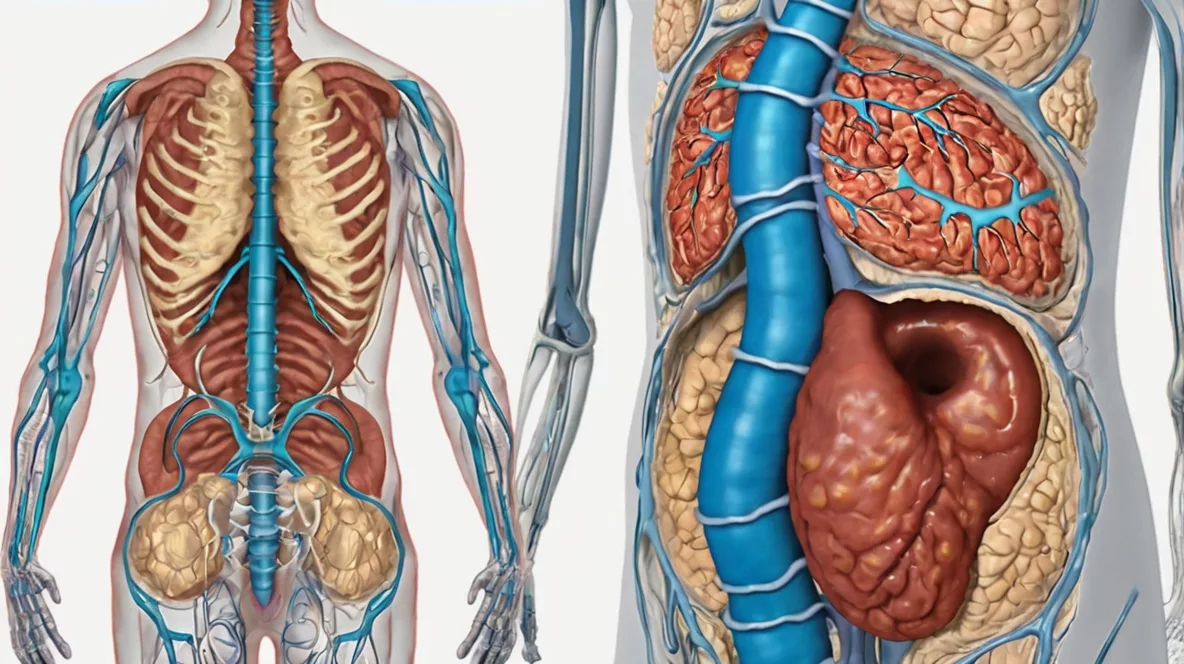
Before diving into the gastroparesis causes, let’s first define gastroparesis. Gastroparesis is a disorder in which the stomach takes too long to empty its contents. It occurs when the stomach’s motility is impaired, usually due to nerve damage or other factors. Normally, your stomach muscles contract to move food through the digestive tract, but in gastroparesis, these contractions are either weak or absent.
This condition can result in food sitting in the stomach for a longer period than normal, causing nausea, bloating, and a feeling of fullness. While it’s not life-threatening in most cases, gastroparesis can significantly affect a person’s daily life, as it interferes with eating, digestion, and overall well-being.
What Causes Gastroparesis?
Several factors can lead to the development of gastroparesis. Understanding these causes can help in managing the condition effectively. While the exact cause is not always clear, the following are common triggers:
1. Damage to the Vagus Nerve
The vagus nerve plays a key role in regulating stomach motility. Damage to this nerve can disrupt the stomach’s ability to empty its contents. This damage can result from diseases like multiple sclerosis (MS), diabetes, and surgery involving the stomach or intestines. In my case, tests have indicated that my digestive transit is good, yet I often experience digestive issues. I suspect that irritable bowel disease (IBD) may contribute to this dysfunction and potentially explain some of my MS-related symptoms.
2. Diabetes
Chronic high blood sugar levels in diabetes can cause damage to the vagus nerve, leading to gastroparesis. In fact, diabetes is one of the most common causes of gastroparesis, with approximately 30% of people with diabetes experiencing some form of the condition. Proper management of blood sugar levels is key to preventing or slowing the progression of gastroparesis in diabetic patients.
3. Surgical Procedures
Certain surgeries, particularly those involving the stomach, oesophagus, or intestines, can cause damage to the vagus nerve or disrupt the stomach’s normal function. These procedures may include weight-loss surgeries, stomach resections, or treatments for gastroesophageal reflux disease (GERD).
4. Medications
Certain medications, especially those that affect the autonomic nervous system or gastrointestinal motility, can cause or worsen gastroparesis. Opioids, anticholinergics, and some antidepressants are known to slow stomach emptying and contribute to the condition.
5. Idiopathic Causes
In many cases, gastroparesis develops without an identifiable cause. When this happens, the condition is referred to as idiopathic gastroparesis. While doctors may not be able to pinpoint the exact trigger, management strategies can still help alleviate symptoms.
6. Other Conditions
Conditions such as Parkinson’s disease, hypothyroidism, scleroderma, and multiple sclerosis (MS) are also known to contribute to gastroparesis. These conditions affect the nerves or muscles that regulate stomach function, making it harder for the stomach to empty properly.
Gastroparesis Symptoms: What to Look For
The symptoms of gastroparesis can vary from mild to severe, depending on the extent of stomach dysfunction. Common symptoms include:
- Nausea and vomiting: Due to the slow movement of food through the stomach, patients may experience nausea and even vomit undigested food hours after eating.
- Bloating and feeling full quickly: Patients often feel full after eating only small amounts of food, or they experience bloating and discomfort.
- Abdominal pain: Some individuals experience pain or discomfort in the abdomen, especially after eating.
- Weight loss: Due to difficulty eating enough and absorbing nutrients, weight loss is common in people with severe gastroparesis.
- Heartburn and acid reflux: Gastroparesis can sometimes exacerbate GERD or lead to reflux symptoms.
It’s important to consult a doctor if you experience any of these symptoms regularly. Early diagnosis and treatment can prevent the condition from worsening.
Gastroparesis Treatment: How to Manage It
There is no one-size-fits-all approach to treating gastroparesis, as treatment plans vary depending on the severity and underlying causes. Common treatments include:
1. Dietary Changes (Gastroparesis Diet)
A gastroparesis diet focuses on eating foods that are easier to digest and don’t place undue stress on the stomach. Common recommendations include:
- Low-fibre foods: Fibre can slow down digestion, so a low-fibre diet is often recommended to avoid constipation and ease digestion.
- Soft or pureed foods: Soft foods like mashed potatoes, soups, and smoothies are easier to digest. Pureeing food can further improve digestibility.
- Smaller, more frequent meals: Eating smaller meals more frequently throughout the day helps the stomach empty more easily.
- Avoiding high-fat foods: Fatty foods slow stomach emptying, so it’s best to limit these in your diet.
2. Medications
Certain medications may be prescribed to help manage the symptoms of gastroparesis, including:
- Prokinetics: These drugs help stimulate stomach contractions and improve motility.
- Anti-nausea medications: These can help alleviate nausea and vomiting caused by the condition.
- Antacids: If acid reflux or heartburn is an issue, antacids may be recommended.
3. Electrical Stimulation Therapy
In some cases, a device called a gastric pacemaker may be implanted to help regulate stomach contractions. This device sends electrical impulses to the stomach muscles to encourage movement and improve digestion.
4. Surgery
In severe cases of gastroparesis, surgery may be considered to improve stomach emptying. Procedures such as gastrostomy tube placement or jejunal feeding tubes are sometimes necessary to provide nutrition if oral intake becomes too difficult.
The best medications for MS flare-ups often include corticosteroids, such as methylprednisolone, to reduce inflammation and speed up recovery.
Gastroparesis Complications: What to Watch Out For
While gastroparesis itself is not typically life-threatening, it can lead to complications such as:
- Malnutrition: Difficulty absorbing nutrients from food can result in deficiencies, weight loss, and malnutrition.
- Dehydration: Vomiting and inadequate food intake can lead to dehydration.
- Blood sugar fluctuations: In people with diabetes, gastroparesis can make blood sugar levels more difficult to control.
Paralysis of the stomach, also known as gastroparesis, can lead to severe digestive issues, including nausea, bloating, and delayed gastric emptying.
Gastroparesis and Multiple Sclerosis
As someone who has been managing multiple sclerosis (MS), I often wonder if my digestive issues are related to MS, particularly since MS can affect the autonomic nervous system, which controls the muscles of the stomach. Multiple sclerosis treatment options may include disease-modifying therapies and managing MS symptoms through medication. However, addressing digestive issues like gastroparesis requires a multidisciplinary approach.
Managing MS Symptoms
People with MS may find it difficult to manage their digestive health due to the disease’s impact on the nervous system. Working with a gastroenterologist and neurologist is key to developing a treatment plan that addresses both gastroparesis and MS.
Frequently Asked Questions
The typical symptoms of gastroparesis include nausea, vomiting, bloating, abdominal pain, and feeling full quickly. Some people also experience weight loss and heartburn.
The most common cause of gastroparesis is diabetes. High blood sugar levels can damage the vagus nerve, which controls stomach muscles, leading to the condition.
Gastroparesis itself is not usually life-threatening. However, complications such as malnutrition or dehydration can negatively affect overall health, so it is important to manage the condition properly.
Gastroparesis may not go away completely, but its symptoms can be managed through dietary changes, medications, and sometimes surgery. The key is to work with your healthcare provider to create an appropriate treatment plan.
Conclusion
Gastroparesis is a complex condition that can have a significant impact on your daily life. Understanding its causes, symptoms, and treatment options is essential for managing the condition. By following a gastroparesis diet, seeking appropriate treatments, and working closely with healthcare professionals, you can alleviate symptoms and improve your quality of life.
Managing the condition often involves a combination of gastroparesis treatment options such as medications, dietary changes, and in severe cases, medical procedures. A well-planned gastroparesis diet, which includes small, low-fat, and low-fiber meals, can help reduce symptoms and improve digestion.